Radiation therapy for eye cancer
Radiation therapy uses high-energy rays or particles to destroy cancer cells.
Radiation therapy is often used to treat eye cancer. Unlike many types of surgery, radiation therapy usually doesn’t affect the eye structure. This can result in a better appearance (how you look) after treatment.
Your healthcare team will use what they know about the cancer and about your health to plan the type and amount of radiation, and when and how it is given.
You may have radiation therapy:
- to kill cancer cells in the eye
- after surgery (called adjuvant therapy) to destroy cancer cells left behind and reduce the risk that cancer will come back
Radiation therapy and chemotherapy may be given during the same time period to treat eye cancer. This is called chemoradiation. Some chemotherapy drugs can help make radiation work better by making cancer cells more sensitive to radiation. Combining chemotherapy and radiation therapy can be more effective than either treatment on its own.
Types of radiation therapy
The following types of radiation therapy are used to treat eye cancer.
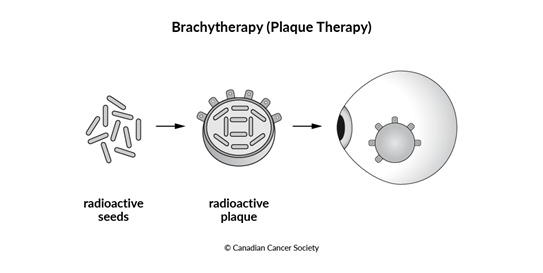
Brachytherapy
Brachytherapy (plaque therapy) is the most common type of radiation therapy used to treat eye cancer. Other names for this treatment for eye cancer include episcleral plaque therapy and ocular brachytherapy.
You’re most likely to have brachytherapy for a small- or medium-sized uveal melanoma tumour (a type of intraocular melanoma) or for squamous cell carcinoma (SCC) of the eye. In brachytherapy, a container shaped like a bottle cap (called a plaque) that contains small radioactive particles (called seeds) is placed on the surface of the eye over the tumour. The radiation kills the cancer cells over time. The plaque is usually made of gold or another metal to protect the tissue around it from exposure to radiation.
You will have surgery to put the plaque in place. It gets sewn into the sclera and is left in place for up to a week. You will have to stay in the hospital while the plaque is on your eye. The plaque gets removed during another surgery.
External beam radiation therapy
During external radiation therapy, a machine directs radiation through the skin to the tumour and some of the tissue around it. External radiation therapy is also called external beam radiation therapy.
External radiation therapy is not used very often for eye cancer. It may be used for melanoma that can’t be treated with brachytherapy, such as a large uveal melanoma tumour or a tumour in the eye that is close to the optic nerve. It is also used for lymphoma that can’t be treated with radioimmunotherapy.
Doctors may use the following external radiation techniques to accurately target the area to be treated and spare as much surrounding normal tissue as possible.
Proton therapy may also be called proton beam therapy. It uses proton beams (positively charged particles) instead of x-ray beams. Protons release more energy after reaching a certain distance and then stop, while x-ray beams release energy before and after they hit their target. So protons cause less damage to tissues they pass through before reaching their target. Proton therapy causes the least amount of damage to nearby normal tissues. A machine called a synchrotron or cyclotron produces the protons. These machines are not available at most centres.
If you have proton therapy for eye cancer, you will have surgery to put metal clips (called tags or tantalum markers) on the surface of your eye. They are sewn onto your sclera to keep them in place and then removed in another surgery.
Stereotactic radiosurgery (SRS)
is a form of
Radioimmunotherapy (RIT)
Radioimmunotherapy (RIT) combines radiation therapy with a
Yttrium-90 (Y-90) ibritumomab tiuxetan (Zevalin) is an RIT drug that is made of a monoclonal antibody that binds to the CD20 protein (ibritumomab) and the radioactive version of yttrium (yttrium-90 or Y-90). Y-90 is attached to the monoclonal antibody in order to deliver radiation therapy directly to the cells the antibody binds to. It is given through a needle into a vein (intravenous).
RIT with Y-90 ibritumomab tiuxetan can be used to treat lymphoma of the eye affecting the uvea or adnexal structures. Very few people will have RIT for eye cancer.
Side effects
During radiation therapy, your healthcare team protects healthy cells in the treatment area as much as possible. Side effects of radiation therapy will depend mainly on the size of the tumour and the specific area being treated, the type of radiation therapy you have, the total dose of radiation and the treatment schedule.
Tell your healthcare team if you have side effects that you think are from radiation therapy. The sooner you tell them of any problems, the sooner they can suggest ways to help you deal with them.
These are common side effects of radiation therapy for eye cancer:
-
cataracts - damage to the blood vessels in the retina (radiation retinopathy)
- increased pressure in the eye (glaucoma)
- vision changes, including blurry vision and loss of vision
- separation of the layers of the retina (detached retina)
- damage to the optic nerve (radiation optic neuropathy)
- dry or teary eyes due to problems with the tear (lacrimal) glands
- swelling and redness around the eye
- loss of eyelashes
- fatigue
- bleeding from the eye
- pain in the eye
Find out more about radiation therapy
Find out more about radiation therapy and side effects of radiation therapy. To make the decisions that are right for you, ask your healthcare team questions about radiation therapy.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
