Results of the 2025 Research Training Awards Master’s Level Competition
The Canadian Cancer Society (CCS) launched the 2025 Research Training Awards in November 2025. The CCS Research Training Awards program aims to support growth and innovation in the next generation of diverse cancer researchers across Canada. This program seeks to build inclusive capacity in all areas of cancer research, while fostering interdisciplinary learning, knowledge translation, mentorship, and patient & community engagement opportunities. By supporting a diverse pool of talented researchers, the program will contribute to reshaping cancer research to be more equitable, inclusive, and impactful. Recognizing that marginalized groups face structural and systemic barriers to inclusion and are underrepresented in the field of cancer research, CCS specifically invited Black and Indigenous trainees to submit applications for the 2025 Master’s level competition in order to positively alter the research landscape.
We are pleased to announce the results of the 2025 Research Training Awards



Funding results of the 2025 Research Training Awards master’s level competition
Funded projects
|
Principal Investigator |
Natnael Abate |
| Funding Amount | $95,000 |
| Grant Duration | 3 years |
| Funding Partner |  |
|
Institution |
University of Alberta |
|
Supervisor |
Michael Hendzel |
|
Short Summary |
Many cancers treatments work by preventing tumour cells from fixing damaged DNA. Over time, that damage builds up, leading to so many mutations that the cells can no longer survive. But some cancers develop ways around these blockers, allowing them to repair damage and resist treatment. Natnael Abate is examining how specific proteins regulate DNA repair and whether we can find new ways of targeting them to prevent cancer treatment resistance. |
|
Problem |
Some cancers become resistant to treatments that block their ability to repair DNA damage. People whose cancers develop this resistance need new treatment options that can effectively target and kill cancer cells. |
|
Solution |
Natnael Abate will use lab techniques to study how certain proteins control the repair of damaged DNA. He aims to learn how these proteins avoid treatments meant to block them – and hopefully find new ways to target the proteins that could lead to more effective treatments. |
|
Impact |
Learning more about the proteins that control DNA damage repair could suggest ways to prevent cancer treatment resistance. It could also reveal weaknesses that can be targeted with new treatments, creating more options for people whose cancer no longer responds to existing therapies. |
|
Principal Investigators |
Adejoke Adekanmbi |
| Funding Amount | $95,000 |
| Grant Duration |
3 years |
| Funding Partner |  |
|
Institution |
University of Calgary |
|
Supervisor |
Oluwabukola Salami |
|
Short Summary |
Black women have lower breast cancer screening rates and higher rates of aggressive breast cancer than other women, leading to poorer outcomes. Adejoke Adekanmbi is studying the barriers that prevent immigrant Black women in Alberta from getting screened and working with communities, healthcare providers and policymakers to make screening more accessible and welcoming. |
|
Problem |
Screening is instrumental for the early detection of breast cancer, which significantly improves outcomes. But immigrant Black women in Canada face barriers that lead to lower screening rates, higher rates of aggressive cancers and worse overall outcomes. |
|
Solution |
Adejoke Adekanmbi will work with immigrant Black women in Alberta, breast cancer survivors, community leaders and healthcare professionals to learn about how they understand and experience screening. She aims to develop ways of making screening programs more accessible and welcoming for this population. |
|
Impact |
Improving screening rates among immigrant Black women could lead to earlier cancer detection, less invasive treatment and better outcomes for these women. Treatment also requires fewer resources when cancer is detected early, reducing the burden on healthcare systems. |
Principal Investigator | Christian Kassa |
| Funding Amount | $65,000 |
| Grant Duration | 2 years |
Institution | University of Windsor |
Supervisor | Lisa Porter |
Short Summary | NEPC is a type of aggressive prostate cancer that is hard to detect and does not respond well to existing treatments. Christian Kassa will study an important cellular process that changes how NEPC cells behave and makes them more aggressive. He will then study if CDK inhibitors can be an effective way of treatment for NEPC, and if using liquid biopsies can help detect NEPC in patients. |
Problem | Neuroendocrine prostate cancer (NEPC) is a type of prostate cancer that is aggressive and difficult to treat and detect. Because the cellular processes in this cancer are not well understood, we currently don’t have much knowledge about how to detect this cancer and how different treatments might work against it or how effective they might be. |
Solution | Christian Kassa will study a cellular process that helps NEPC cells survive and resist treatment and detection. He will look at how drugs called CDK inhibitors affect NEPC cells and metastasis to see whether they might be an effective treatment option. Christian will also help develop a non-invasive way to detect NEPC tumors in patients by studying liquid biopsy samples. |
Impact | At the moment, there’s no standard way of treatment and detection for NEPC. If this research shows that CDK inhibitors can kill NEPC cells and shrink tumours, it will suggest a new approach to treating these cancers that could improve outcomes for people with NEPC. Also, discovering better ways to detect NEPC earlier could help doctors respond faster and improve patient care. |
|
Principal Investigator |
Johnathon Lucas |
| Funding Amount | $65,000 |
| Grant Duration |
2 years |
| Funding Partner |
 |
|
Institution |
University of Manitoba |
|
Supervisor |
Cédric Tremblay |
|
Short Summary |
Many children and adults who are treated for T-cell leukemia see their cancer return after chemotherapy. A protein called STAT5 can help cancer cells survive treatment, but the drugs that currently target it are too toxic to be given to people with leukemia. Johnathon Lucas is looking at the processes STAT5 controls with the goal of finding new ways to treat T-cell leukemia. |
|
Problem |
T-cell leukemia is an aggressive cancer that often comes back after chemotherapy. Sometimes, a protein called STAT5 helps leukemia cells survive treatment so that the cancer can return – but the drugs that target STAT5 are too toxic for use in people with leukemia, so alternative treatments are needed. |
|
Solution |
Johnathon Lucas will look at which cellular processes STAT5 controls and what else is involved in these processes. Understanding these processes could reveal new and less toxic therapies to treat T-cell leukemia. |
|
Impact |
T-cell leukemia comes back after treatment in 1 in 5 children and 3 in 5 adults. More than half of T-cell leukemia cases involve cell processes that STAT5 controls. Finding ways to target STAT5-controlled cell processes could lead to new treatments that improve outcomes for people with these leukemias. |
|
Principal Investigator |
Diery-Leando Saint-Vil |
| Funding Amount | $32,500 |
| Grant Duration |
1 year |
|
Institution |
McGill University |
|
Supervisors |
Lysanne Campeau & Maurice Anidjar |
|
Short Summary |
Some prostate cancers can be treated using focal therapy, which targets and destroys cancer cells without damaging healthy cells. Right now, focal therapy is effective in less aggressive cancers but doesn’t work as well in more aggressive prostate cancer. Diery-Leando Saint-Vil is studying how focal therapy affects cancer cells with the goal of making it more effective as a treatment for aggressive prostate cancer. |
|
Problem |
Focal therapy is a type of prostate cancer treatment that works well to target and destroy cancer cells without harming healthy cells – leading to fewer side effects than surgery or radiation. At the moment, it is only effective against less aggressive cancers, which means that people with more aggressive prostate cancer cannot benefit from this type of treatment. |
|
Solution |
Diery-Leando Saint-Vil will study proteins called neurotrophins that may help prostate cancer cells survive and resist treatment. He will investigate whether blocking these proteins can weaken cancer cells and make them more susceptible to focal therapy. |
|
Impact |
Finding new ways of weakening cancer cells could make focal therapy effective in people with aggressive prostate cancer. This could provide a new treatment option for these people that is less invasive and has fewer side effects, offering better quality of life during and after treatment. |
|
Principal Investigator |
Joanna Mbuya Malaïka Mutombo |
| Funding Amount | $65,000 |
| Grant Duration |
2 years |
|
Institution |
CHUL - Centre hospitalier de l'Université Laval |
|
Supervisors |
Lynn R. Gauthier |
|
Short Summary |
Some types of chemotherapy can lead to neuropathy, a side effect that causes numbness, pain, burning or tingling feelings in the limbs. Older people may be more at risk for neuropathy than younger people, and the condition may behave differently in people of different ages. Joanna Mbuya aims to understand how neuropathy looks in older and younger people so that it can be better managed. |
|
Problem |
Many people treated with chemotherapy drugs called taxanes develop neuropathy. This can cause a wide range of symptoms, including pain, numbness, tingling, burning, cramping, shocks, dizziness, balance problems and many more. We don’t yet understand how neuropathy changes with age or why it looks different in people of different ages. |
|
Solution |
Joanna Mbuya will assess people aged 18 to 59 and people aged 60 and over who have been treated with taxanes. She will collect information on people’s symptoms including pain and other unusual sensations with physical tests, surveys and more to understand what neuropathy is like at different ages. |
|
Impact |
There are very few treatment options for neuropathy. Understanding more about the condition and how it manifests in younger and older people could help predict what neuropathy may look like in people who are treated with taxanes, how long it may last and how to improve quality of life for people with neuropathy. |
Expert Review Process for the Research Training Awards
8 full applications were received and underwent review by an expert panel comprised of national scientific experts, as well as patient/survivor/caregiver reviewers with lived experience. 6 have been approved for funding – corresponding to a 75% success rate. These awards, with support from generous funding partners, total more than $400k in funding over the full term of these awards.
Investment by research goal
Results by research area
Results by province of trainee’s institution

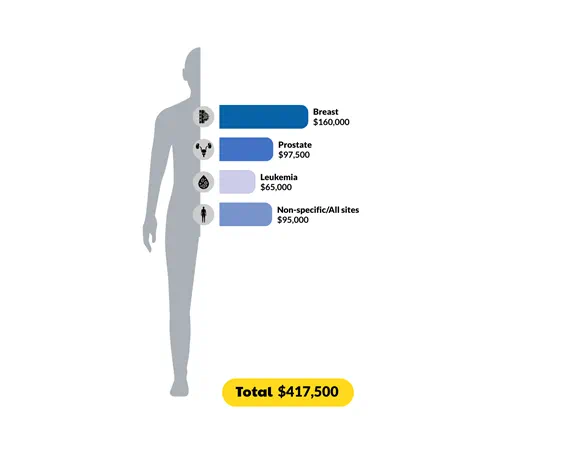
Investment by cancer site