Stages of uterine cancer
Staging describes or classifies a cancer based on how much cancer there is in the body and where it is when first diagnosed. This is often called the extent of cancer. The healthcare team uses various tests and procedures to find out the size of the tumour, which parts of the organ have cancer, whether the cancer has spread from where it first started and where the cancer has spread. Doctors use the stage to plan treatment and estimate the outcome (prognosis).
The most common staging system for uterine cancer is the International Federation of Gynecology and Obstetrics (FIGO) system. For uterine cancer, there are 4 stages. Often the stages 1 to 4 are written as the Roman numerals I, II, III and IV. Generally, the higher the stage number, the more the cancer has spread.
In most cases, uterine cancer is staged surgically, which means that the stage is determined after surgery to remove the cancer. The tissue removed during surgery is looked at in a lab and the information collected is combined with the results of tests done during diagnosis. This gives the healthcare team information on aspects of the cancer that are used to help stage it, including:
- which parts of the uterus are affected by cancer
- if the cancer has grown into tissues around the uterus
- if the cancer has spread to the lymph nodes
- if the cancer has spread to distant sites (called metastasis)
- the grade
- the molecular subtype
- the cellular (pathologic) type of endometrial carcinoma
In cases when you can’t have surgery or want to conceive (get pregnant), you won’t have uterine cancer staged surgically. Instead, an endometrial biopsy may be done during diagnosis to help stage the cancer and guide treatment. Your healthcare team will talk to you about how cancer staged using a biopsy differs from cancer that is surgically staged.
Staging uterine cancer is complex. You may want to ask your healthcare team to explain it to you in a way you understand or to answer any questions. Find out more about staging cancer.
The following stages are used for endometrial carcinoma and uterine
Molecular subtyping
Molecular subtype is a classification given to endometrial carcinoma based on whether it has certain genetic mutations. During the staging process, tests are done in the lab to look for these mutations in the tissue removed during biopsy or surgery. According to the results of these tests, doctors assign the cancer to 1 of the 4 molecular subtypes, including:
- POLEmut– DNA polymerase epsilon mutated
- MMRd– mismatch repair deficient
- p53abn– abnormal tumour protein 53
- NSMP– non-specific molecular profile
Find out more about the molecular subtypes of endometrial carcinoma.
When describing the stage your doctor may also use the terms non-aggressive and aggressive. These terms are a classification given to the cancer type based on how the cancer grows and its prognosis. Doctors consider the type of cancer you have and whether it is aggressive or not when staging endometrial carcinomas.
Non-aggressive means the cancer is slow growing and is less likely to spread. Types of non-aggressive endometrial carcinoma include low-grade (grade 1 or 2) endometrioid adenocarcinoma.
Aggressive means the cancer is faster growing and more likely to spread. Types of aggressive endometrial carcinoma include:
- high-grade endometrioid adenocarcinoma
- serous carcinoma
- carcinosarcoma
- clear cell carcinoma
- mixed carcinoma
- undifferentiated carcinoma
- mesonephric-like adenocarcinoma
- gastric-type carcinoma
Stages for endometrial carcinoma
The following stages are used for endometrial carcinoma. If you have a different type of uterine cancer, talk to your doctor about staging. The stages may be different based on features and specific information for the type of cancer.
Stage 1
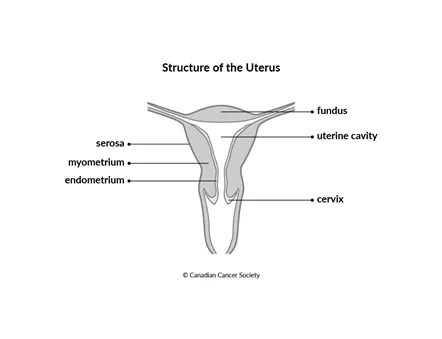
Stage 1A is a non-aggressive type of endometrial carcinoma. It is only in the inner lining of the uterus (called the endometrium), is only an endometrial polyp, or has grown less than halfway into the muscle layer of the uterus wall (called the myometrium). Or the tumour is a low-grade carcinoma. It is only in the uterus or ovaries.
Stage 1A-mPOLEmut means the molecular subtype of the cancer is POLEmut. The tumour has not grown outside of the uterus and cervix.
Stage 1B is a non-aggressive type of endometrial carcinoma. It has not grown outside the uterus and cervix.
Stage 1C is an aggressive type of endometrial carcinoma or a uterine carcinosarcoma. It is only in the endometrium or is only an endometrial polyp.
Stage 2
Stage 2A is a non-aggressive type of endometrial carcinoma. It has spread into the cervical stroma, the deepest layer of the cervical wall.
Stage 2B is a non-aggressive type of endometrial carcinoma. There is lymphovascular invasion by cancer cells.
Stage 2C is an aggressive type of endometrial carcinoma or a uterine carcinosarcoma. It has grown into the myometrium.
Stage 2C-mp53abn means the molecular subtype of the cancer is p53abn. The tumour has not grown beyond the endometrium, myometrium and cervix.
Stage 3
Stage 3A is a high-grade carcinoma or a uterine carcinosarcoma. It has spread to the ovaries or fallopian tubes. Or the tumour has grown through the outer surface of the uterus (called the uterine serosa) or into the space right below it (called the subserosa).
Stage 3B has spread into the vagina or grown outside the uterus into the connective tissues that surround the uterus and cervix (called the parametrium). Or the cancer has grown into the part of the peritoneum lining the inside of the pelvis and has not grown past the pelvic organs into the part lining the abdomen.
Stage 3C has spread to lymph nodes in the pelvis (called pelvic lymph nodes) or to lymph nodes around the aorta (called para-aortic lymph nodes).
Stage 4
Stage 4A has spread into the lining of the bladder or intestines.
Stage 4B has spread into the peritoneum lining the abdomen.
Stage 4C has spread to other lymph nodes in the abdomen beyond the pelvic and para-aortic lymph nodes. Or the cancer has spread to other parts of the body, such as the lungs, the liver or bones (called distant metastasis or metastatic cancer).
Recurrent uterine cancer
Recurrent uterine cancer means that the cancer has come back after it has been treated. If it comes back in the same place that the cancer first started, it’s called a local recurrence. If it comes back in tissues or lymph nodes close to where it first started, it’s a called regional recurrence. It can also come back in another part of the body that is further away from where it first started. This is called distant metastasis or distant recurrence.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
