Surgery for pancreatic cancer
Surgery is a medical procedure to examine, remove or repair tissue. Surgery, as a treatment for cancer, means removing the tumour or cancerous tissue from your body.
Some people with pancreatic cancer have surgery. The type of surgery you have, or whether you can have surgery at all, depends on aspects of the cancer including its stage, if it has spread, and the size and location of the tumour in the pancreas. When planning surgery, your healthcare team will also consider other factors, such as your age, overall health and any other treatments you may have had for pancreatic cancer.
Surgery may be the only treatment you have or it may be used along with other cancer treatments. You may have surgery to:
- try to completely remove the tumour
- reduce pain or ease symptoms (called palliative surgery)
Sometimes a tumour may look
The following types of surgery are used to treat pancreatic cancer.
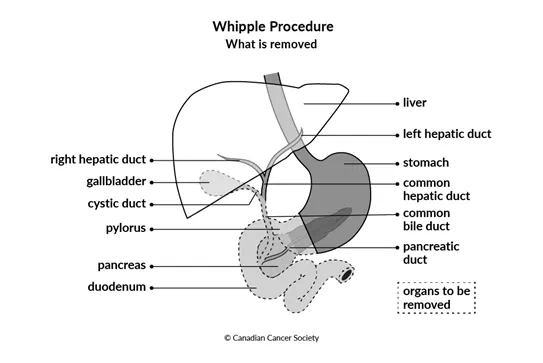
Whipple procedure
A Whipple procedure (pancreaticoduodenectomy) is the most common surgery to treat pancreatic cancer. It is used to treat resectable pancreatic cancer that's in the head of the pancreas. A Whipple procedure removes:
- the head of the pancreas
- the pancreatic duct
- the gallbladder
- part of the common bile duct
- the part of the stomach that connects to the small intestine (pylorus)
- the first part of the small intestine (duodenum)
- lymph nodes around the pancreas
- blood vessels around the pancreas (if necessary)
After removing these organs, the surgeon will reconstruct the digestive tract. They will typically reattach the remainder of the small intestine to the common hepatic duct (the tube that normally carries bile from the liver into the bile duct), the remainder of the stomach and the remainder of the pancreas.
A Whipple procedure and reconstruction is usually done by open surgery, but it
can also be done by
The Whipple procedure is a long and complex surgery that can only be done by very experienced surgeons. A Whipple procedure may not be available at all treatment centres or hospitals.
Find out more about the Whipple procedure.
Modified Whipple procedure
The modified Whipple procedure (also called a pylorus-preserving pancreaticoduodenectomy) removes all of the same organs as the Whipple procedure except for the pylorus.
After removing these organs, the surgeon will reconstruct the digestive tract. They will reattach the common hepatic duct, the pylorus and the remainder of the pancreas to the remainder of the small intestine.
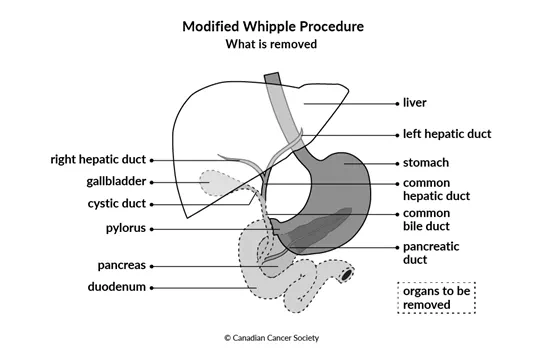
The kind of Whipple procedure done to remove a pancreatic tumour is based on the surgeon's opinion, the size of the tumour and its location in the pancreas. The outcomes and side effects of the Whipple procedure and modified Whipple procedure are typically the same.
Find out more about the modified Whipple procedure.
Distal pancreatectomy
A distal pancreatectomy is done for resectable pancreatic tumours in the body or tail of the pancreas. This surgery removes:
- the tail (and sometimes part of the body) of the pancreas
- lymph nodes around the pancreas
- the spleen
- blood vessels around the pancreas (if necessary)
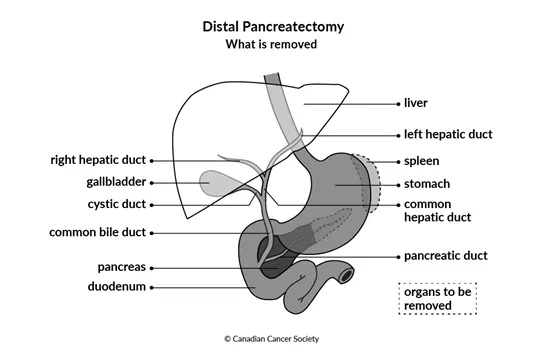
If you have a distal pancreatectomy, you will need to have certain vaccinations to replace the function of the spleen.
Total pancreatectomy
A total pancreatectomy (also called an en-bloc pancreaticoduodenectomy) is used to treat resectable pancreatic cancer that cannot be removed with a Whipple procedure or distal pancreatectomy. It is rare to have a total pancreatectomy.
A total pancreatectomy removes:
- the pancreas
- the gallbladder
- part of the common bile duct
- the part of the stomach that connects to the small intestine (pylorus)
- the first part of the small intestine (duodenum)
- the spleen
- lymph nodes around the pancreas
- blood vessels around the pancreas (if necessary)
After removing these organs, the surgeon will reconstruct the digestive tract. They will reattach the remainder of the small intestine to the common hepatic duct (the tube that normally carries bile from the liver into the bile duct) and the remainder of the stomach.
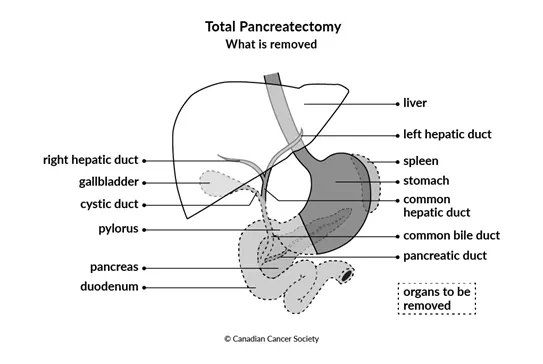
Because there is no remaining pancreas after a total pancreatectomy, you will need to take medicines (including insulin and digestive enzyme replacements) for the rest of your life to replace the essential functions of the pancreas if you have this surgery. You will also need to have certain vaccinations to replace the function of the spleen. Find out more about supportive care for pancreatic cancer.
Palliative surgery
For unresectable or recurrent pancreatic cancer, you may be offered a palliative procedure.
Tumours in the head of the pancreas often block the common bile duct or the duodenum. Palliative procedures are used to control symptoms caused by these blocks and improve quality of life. The procedure done depends on several factors including your predicted prognosis, what part of the pancreas the tumour is in and your overall health.
Most people will have the following palliative procedures
Stent placement
You may be offered a stent if your bile duct or duodenum is blocked by a tumour in the head of the pancreas that cannot be removed.
A stent is a small metal or plastic tube placed into the bile duct or duodenum that helps keep the duct or intestine open and allows for things to flow through them normally. The most common way to place a stent to relieve a bile duct or duodenal blockage is through an ERCP (endoscopic retrograde cholangiopancreatography). In some cases, stents are placed percutaneously or during another surgery instead.
Bypass procedures
If you have a blockage of the bile duct or duodenum caused by a tumour in the head of the pancreas, you may be offered a bypass procedure. A bypass procedure creates a path around the blockage so food or bile can flow normally into the small intestine.
A biliary bypass creates a path for bile to flow around a blockage in the bile duct. The path that the surgeon creates depends on the location of the blockage. A biliary bypass is done through open surgery.
A biliary bypass is used far less often than stent placement. It may be preferred to a stent:
- for patients expected to live with unresectable pancreatic cancer for one or more years
- if the surgeon wants to treat the nerves around the pancreas to relieve pain
- to avoid having to do multiple procedures when a surgery was started or needed for another reason
A gastric bypass( also called a gastrojejunostomy, or enteric bypass) creates a path for partially digested food from the stomach to flow around a blockage in the duodenum. The surgeon connects the pylorus to the jejunum (the second segment of the small intestine). A gastric bypass is done through open surgery.
Some people will have both a gastric bypass and bile duct stent.
Side effects
Side effects of surgery will depend mainly on the type of surgery, what tissues are removed and your overall health. Tell your healthcare team if you have side effects that you think are from surgery. The sooner you tell them of any problems, the sooner they can suggest ways to help you deal with them.
Surgery for pancreatic cancer may cause these side effects:
- pain
- indigestion or difficulty digesting certain foods
- difficulty absorbing nutrients (malabsorption)
- weight loss
- bowel changes, such as diarrhea, constipation, or stools that are large, pale or light-coloured, smell very foul and float in the toilet
-
delayed gastric emptying - dumping syndrome
- leaking of bile, stomach acid or pancreatic juices from the site where the remainder of the pancreas, stomach, bile duct and small intestine were reattached during surgery
-
a
fistula between your pancreas and abdominal cavity (the hollow part in the abdomen) - diabetes
Find out more about surgery
Find out more about surgery and side effects of surgery. To make the decisions that are right for you, ask your healthcare team questions about surgery.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
