Surgery for breast cancer
Surgery is a medical procedure to examine, remove or repair tissue. Surgery, as a treatment for cancer, means removing the tumour or cancerous tissue from your body.
Most people with breast cancer have surgery. The type of surgery you have depends mainly on the size and location of the tumour, the size of the breast, if the cancer has spread to the lymph nodes and any other treatments you have already had for breast cancer. When planning surgery, your healthcare team will also consider other things, such as your overall health and the type of surgery you want to have.
Surgery is commonly used along with other cancer treatments. You may have surgery to:
- completely remove the tumour
- check if the cancer is in the lymph nodes
- remove cancer that comes back in the breast (called a local recurrence)
- remove one or both breasts if you have a high risk of developing breast cancer (called a prophylactic mastecomy)
- reshape the breast after the cancer has been removed (called breast reconstruction)
Chemotherapy may be given before surgery (called neoadjuvant chemotherapy) to shrink a large tumour to make it easier to remove.
Side effects of surgery will depend mainly on the type of surgery and your overall health. Tell your healthcare team if you have side effects that you think are from surgery. The sooner you tell them of any problems, the sooner they can suggest ways to help you deal with them.
The following types of surgery are used to treat breast cancer. Your healthcare team will discuss the options with you to help you decide which surgery is right for you. The type of surgery you choose may affect other treatments you have before or after surgery. Find out more about choosing the breast surgery that is right for you.
Breast-conserving surgery (BCS)
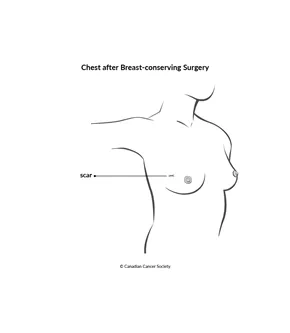
Breast-conserving surgery (BCS) is sometimes called a lumpectomy. This type of surgery keeps, or conserves, as much of the breast as possible. In most cases, BCS will be followed by radiation therapy.
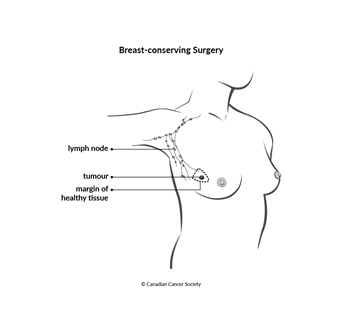
BCS may be offered if the surgeon can safely remove the breast tumour along with an area of tissue surrounding the tumour (called a margin of tissue) and still leave enough tissue so the breast looks natural. The breast looks and feels a little different after BCS, but often the changes are not very noticeable. After surgery, the breast is smaller, slightly different in shape and slightly firmer.
BCS is most often used to treat ductal carcinoma in situ (DCIS) and early-stage breast cancer.
The surgeon usually removes some lymph nodes from under the arm as well during BCS.
How BCS is done
BCS is done in a hospital with either a local or general
After removing the abnormal area or tumour, the surgeon closes the skin with stitches or special staples. A bandage or dressing is placed over the wound. The healthcare team will remove the stitches or staples once the incision heals. Some types of stitches dissolve on their own.
The healthcare team sends the removed breast tissue to a lab. A
A negative (clear) margin means there are no cancer cells in the edges of the removed tissue.
A positive margin means there are cancer cells in the edges of the removed tissue.
If there is a positive margin, the surgeon will need to remove more tissue because the cancer cells left behind can grow into another tumour or spread. Another BCS is done to remove more breast tissue from the same surgical site, or a mastectomy is done to remove all of the breast tissue.
Side effects of BCS
BCS may cause these side effects:
- bleeding
- infection
- pain or tenderness in the breast
- swelling of the breast that may be temporary (for example, a collection of fluid that needs to be drained)
- a change in the shape of the breast
- scar tissue or dimple that forms where the tissue was removed
- lymphedema if lymph nodes were also removed
- nerve pain in the chest wall, armpit or arm that doesn't go away (called post-mastectomy pain syndrome, or PMPS)
- changes to body image and self-esteem
Mastectomy
A mastectomy removes all of the breast. It may be done:
- to treat tumours that are large compared to the size of the breast
- when the cancer is in more than one area of the breast
- if there are positive margins after BCS
- if you can't have BCS or the radiation therapy that usually follows BCS
- if the cancer comes back, or recurs, in the breast after BCS and radiation therapy
- if you choose to have a mastectomy instead of BCS
- to treat inflammatory breast cancer
Types of mastectomy
The following types of mastectomy may be offered.
Total mastectomy
A total mastectomy removes all of the breast and the tissue that covers the chest muscles (called the pectoral fascia). The lymph nodes, nerves and muscles in the chest are left in place. The nipple may or may not be removed. A total mastectomy may also be called a simple mastectomy.
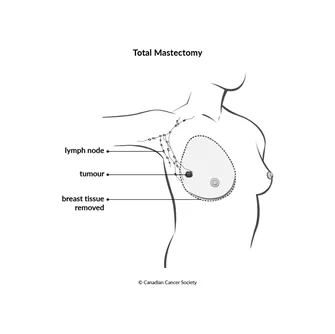
A skin-sparing mastectomy is like a total mastectomy except that the surgeon doesn’t remove the skin that covers the breast. It is an option if you plan to have breast reconstruction at the same time as the surgery and the breast reconstruction can be done with very little scarring.
A
double (bilateral) mastectomy
is a surgery – usually a total mastectomy – that removes both breasts.
It is sometimes done to prevent breast cancer in people who have a very
high risk of the disease, such as people with
Modified radical mastectomy
A modified radical mastectomy removes all of the breast, the nipple, the tissue that covers the chest muscles and most or all of the lymph nodes in the armpit. Nerves and muscles are usually left in place.
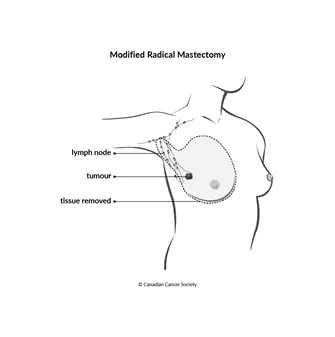
This type of mastectomy is used for breast cancer that has spread to the lymph nodes. It is also used to treat inflammatory breast cancer.
A radical mastectomy is surgery that removes more muscle, lymph nodes and other tissues than a modified radical mastectomy. A radical mastectomy is very rare.
How a mastectomy is done
A mastectomy is done in a hospital while you are under anesthesia– usually a general anesthetic.
After removing the breast and other tissues, the surgeon may place plastic or rubber tubes in the area where the breast was removed or under the arm. These tubes, or drains, remove blood and lymph fluid that collect during healing.
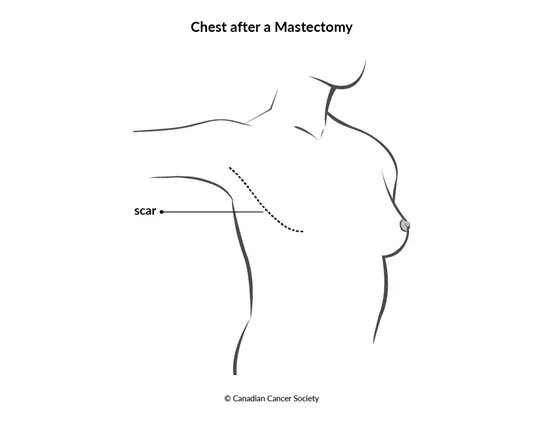
The surgeon closes the skin with stitches or special staples. A bandage or dressing is placed over the wound.
Side effects of a mastectomy
A mastectomy may cause these side effects:
- bleeding
- infection
- pain
- swelling of the area where the tissue was removed
- a buildup of blood or fluid in the wound
- scarring of the tissue
- problems moving your arm or shoulder
- numbness in the chest
- nerve pain in the chest wall, armpit or arm that doesn't go away (called post-mastectomy pain syndrome, or PMPS)
- lymphedema if lymph nodes were also removed
- changes to body image and self-esteem
Lymph node surgery
As part of the staging process for breast cancer, the surgeon removes lymph nodes so they can be checked to see if they have cancer in them.
Sentinel lymph node biopsy
A sentinel lymph node biopsy (SLNB) removes the sentinel node to see if there is cancer in it. The sentinel lymph node is the first lymph node in a chain or cluster of lymph nodes that gets lymph fluid from the area around a tumour. Cancer cells will most likely spread to the sentinel lymph node. There may be more than one sentinel lymph node, depending on where the lymph vessels carry lymph fluid from the area around the tumour.
If you are younger than 70 years old and don't have any other significant health problems, you will have an SLNB to see if the cancer has spread to the lymph nodes and find out if early-stage breast cancer is stage 1 or stage 2A.
An SLNB is not usually needed if you are 70 or older and have early-stage breast cancer that is hormone-receptor positive and HER2 negative and has not spread to the lymph nodes.
If you have chemotherapy before surgery, you will have an SLNB at the time of your breast surgery.
If the sentinel lymph node doesn’t contain cancer, no more lymph nodes need to be removed. If the sentinel node does contain cancer or the doctors can’t find the sentinel node, you may be given a choice of an axillary node dissection or radiation therapy to the area of the axillary lymph nodes.
Find out more about a sentinel lymph node biopsy.
Axillary lymph node dissection (ALND)
An axillary lymph node dissection (ALND) removes the lymph nodes under the arm (called the axillary lymph nodes). It is the type of lymph node surgery most commonly done if breast cancer has spread to the lymph nodes.
If you were diagnosed with breast cancer in the lymph nodes and the cancer did not respond well to chemotherapy, you will have an ALND at the time of your breast cancer surgery.
Find out more about an axillary lymph node dissection.
Side effects of lymph node surgery
Lymph node surgery may cause these side effects:
- bleeding
- infection
- pain
- lymphedema (more common after an ALND than after an SLNB)
- numbness under the arm
- limited shoulder and arm movement
After breast cancer surgery
Breast cancer surgery may be done as an outpatient procedure or you may have to stay in the hospital. How long you stay in the hospital will depend on the type of surgery, your general health and how you feel after the surgery.
If the surgeon placed drains during surgery, they may need to stay in place when you go home. The healthcare team will tell you how to take care of the surgical area and the drains at home. The drains are removed when there is little drainage from them.
The healthcare team will remove stitches or staples once the incision has healed. Some types of stitches dissolve on their own.
You may also be given information on how to manage pain and rehabilitation exercises to do after you recover from the surgery. Find out more about supportive care for breast cancer.
Find out more about surgery
Find out more about surgery and side effects of surgery. To make the decisions that are right for you, ask your healthcare team questions about surgery.
Choosing the breast surgery that is right for you
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
