Lymphedema
Lymphedema is swelling that happens when lymph can’t flow normally and builds up in the soft tissues of a limb. Lymphedema usually happens in parts of the body where lymph nodes have been removed or damaged by cancer treatment. These areas include the underarm (axilla), neck, groin and pelvis. The risk of lymphedema increases with the number of lymph nodes that are affected. Lymph nodes are a part of the lymphatic system.
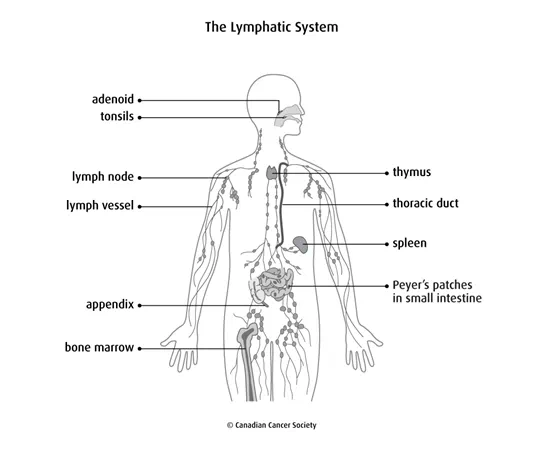
Lymph is a clear, yellowish fluid that contains nutrients, lymphocytes (a type of white blood cell) and antibodies. Lymph travels throughout the body in lymph vessels. Lymph nodes sit along the lymph vessels. Their job is to filter the lymph.
Causes
Lymphedema can be caused by:
- surgery that removes lymph nodes (called lymph node dissection)
- radiation therapy to lymph nodes
- cancer that spreads (metastasizes) to the lymph nodes
- an infection or inflammation that damages lymph vessels
- injury to the lymph nodes
People who have lymph nodes under the arm removed as part of breast cancer treatment are at risk of developing lymphedema in that arm. Lymphedema can develop in the legs after treatment for different types of cancer including lymphoma and melanoma as well as uterine, prostate, vulvar and ovarian cancers.
Symptoms
Symptoms can vary depending on how severe the lymphedema is. Symptoms of lymphedema include:
- swelling in an arm or leg, which may include the fingers or toes
- feeling of fullness, puffiness or heaviness in the arm, leg or genital area
- aching or burning feeling in the limb
- tight or warm feeling in the skin of the arm, leg or genital area
- trouble moving a joint in the arm or leg
- hardening or thickening of the skin
- feeling that jewellery or clothes are tight
Diagnosis
Diagnosis is the process of finding out the cause of a health problem. Your doctor will try to find the cause of lymphedema and will ask questions about your health history, including past illnesses and treatments. Your doctor will also do a physical exam because lymphedema usually has obvious signs. This may include measuring the distance around (circumference of) the swollen arm or leg and comparing it to the other arm or leg.
Doctors may give lymphedema a stage or grade based on how severe the symptoms are. This includes how the skin reacts to the touch, if swelling goes down when the limb is elevated and if the skin is scarred or feels different. This information is used to plan treatment.
You may also have the following imaging tests to help your doctor find the cause of lymphedema:
Preventing and managing lymphedema
Treatment of lymphedema depends on the cause. Your healthcare team will suggest ways to prevent lymphedema or help manage it if you do get it.
It is important to stop lymphedema from getting worse, even when you have some permanent damage to the lymph system. Lymphedema in your arm or leg can lead to serious complications such as a bacterial infection of the skin (called cellulitis) or an infection of the lymphatic vessels (called lymphangitis).
Treatments for lymphedema are based on how severe it is, and they aim to:
- lessen the swelling
- relieve pain
- stop lymphedema from getting worse
- prevent an infection
- improve movement and use of the arm or leg
Skin care
Taking good care of your skin can help prevent an infection. It can also prevent lymphedema from getting worse and keep your skin from drying and cracking. Any damage to the skin, such as burns, cuts, blisters and cracks, can lead to an infection.
Keep your skin clean by bathing regularly. Be sure to test the water temperature because limbs with lymphedema may not feel temperatures as well as normal. Avoid extreme hot or cold such as heating pads or cold packs. Heat can make lymphedema worse so check with your healthcare team before you use saunas, steam baths or hot tubs.
Wear sunscreen to avoid sunburns, especially to the affected limbs. Wear long sleeves and long pants if you need to be in the sun.
Keep your hands, feet and cuticles soft by using lotion at least once a day. Clip toenails straight across and file your fingernails. Do not cut or tear cuticles. Keep your feet clean and wear cotton socks. Wear comfortable and supportive shoes. Change your socks as soon as possible if they get wet.
Wear loose-fitting jewellery and clothing that doesn’t have tight elastic cuffs or waistbands.
Protect yourself when you do activities that may cause damage to the skin. Wear gloves when you garden or cook. Use a thimble when sewing. Use an electric razor for shaving. Avoid walking barefoot, especially outside.
Avoid pet scratches and insect bites. Use insect repellant when outside.
Treat cuts or burns on the limb quickly. Clean the area, cover it with an antibacterial cream and apply a clean bandage. Change the bandage as often as necessary to avoid getting an infection.
Don’t put pressure on the arm or leg. For example, don’t carry a purse on the treated side and don’t cross your legs or ankles when sitting or lying. Avoid having blood pressure measured on the affected arm. If lymph nodes were removed from under both arms, switch arms each time you have your blood pressure checked.
Avoid having needle sticks of any type in the affected limb. This includes having a blood sample taken, an intravenous (IV), an injection and acupuncture on the affected limb or in affected areas.
Compression garments
Compression garments are also called pressure garments, compression sleeves and lymphedema sleeves or stockings. They are made of elasticized fabric. They put a controlled amount of pressure on different parts of the arm or leg to help move lymph and keep it from building up. The garment may need to be worn all day (during waking hours), when working and when you exercise. It is important to use compression garments during air travel because lymphedema can become worse at high altitudes.
Compression garments should only be worn when a doctor or physiotherapist recommends them. They are fitted to each person and you will be told how and when to wear them.
Exercise
You may be given stretching exercises to help loosen the tissues in certain areas or move lymph out. Gentle exercise helps lymph circulate (flow) and reduces swelling. Exercise also increases blood flow to the muscles, which can increase the amount of lymph. Check with a healthcare professional, such as a physiotherapist, before beginning an exercise routine that includes vigorous, repetitive activities. You should wear a compression garment during exercise if you have lymphedema.
Maintain a healthy body weight
Extra body weight is a risk for developing lymphedema. It can also make lymphedema harder to control. You can lower your risk by having a healthy body weight. Eating well and being physically active can help. Losing weight may lessen lymphedema.
Bandages
Bandaging or wrapping a swollen limb helps the lymph vessels move lymph along. After lymph is moved out of a swollen limb, wrapping or bandaging the limb may help prevent fluid from building up in the area again. Talk to your physiotherapist about the proper way to wrap the limb.
Elevation
Keeping the affected limb elevated (raised up), may help the lymph drain from the limb and lessen the swelling. But keeping an arm or leg elevated for a long period of time is often not possible.
Manual lymph drainage (MLD)
Manual lymph drainage (MLD), also called manual lymph therapy (MLT), is a special kind of light massage. It is usually done by a massage therapist or physiotherapist with special training in treating lymphedema. Your therapist can also teach you how to do it yourself.
During MLD, you or your therapist lightly rubs, taps and strokes the soft tissues of the body. This improves drainage from the limb by clearing out the main lymphatic pathways.
Complex decongestive therapy (CDT)
Complex decongestive therapy (CDT), also called complex physiotherapy (CPT), is a combination of manual lymph drainage, skin care, compression bandaging, exercises and compression garments. These therapies are managed by a massage therapist or physiotherapist with special training. The therapist gives many treatments over a short time to help clear most of the swelling. Then you can continue the program at home to keep the swelling down.
Compression device
Compression devices are pumps connected to a sleeve that wraps around the arm or leg. The device pumps air into the sleeve on and off during a timed cycle. This pumping action may help move fluid through the lymph vessels and veins so that it doesn’t build up. These devices may be helpful when used along with another type of therapy. They should be supervised by a trained professional because too much pressure could damage lymph vessels near the skin surface.
Laser therapy
Laser therapy may help to lessen lymphedema and skin hardness. A therapist specially trained in using lasers uses a hand-held device to aim low-level laser beams at the area with lymphedema.
Liposuction
Liposuction is a surgical procedure that sucks out fat deposits from specific areas of the body. It may be done to treat lymphedema in the area under the chin (called submental lymphedema). Fluid can build up in this area following treatment for head and neck cancer.
Liposuction has also had good results in lowering the amount of fluid in a limb in people with severe lymphedema related to breast cancer treatment. It is most effective when the fluid builds up in mostly fat and fibrous tissue. But if you have liposuction to treat lymphedema, you’ll need to wear a compression sleeve 24 hours a day for a long time and maybe forever.
Lymphovenous bypass
A lymphovenous bypass is new surgery used to treat some people with lymphedema. It does not cure lymphedema but it can help to lessen the swelling permanently. It is only done by specially trained surgeons. It involves attaching lymphatic vessels to nearby veins in the area where lymph nodes have been removed.
Lymph node graft
A lymph node graft is surgery being studied in clinical trials to treat people with lymphedema. It moves lymph nodes, usually from around the collar bone or neck area, to the area where lymph nodes have been removed.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
