Bowel resection
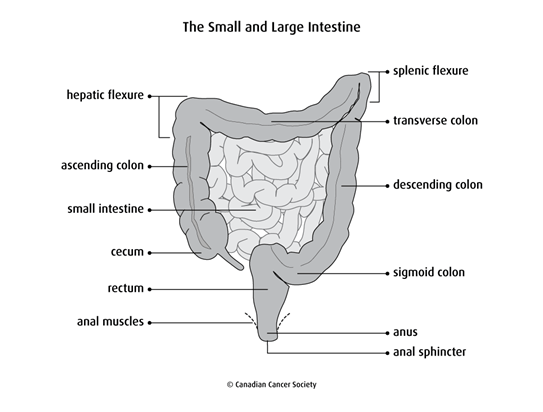
Bowel resection is surgery to remove part of the small intestine, large intestine or both. The large intestine includes the colon, rectum and anus. Depending on which parts of the intestine are removed, a bowel resection may also be called:
- a small bowel resection or small intestine resection
- a large bowel resection or large intestine resection
- a colectomy
Why a bowel resection is done
A bowel resection is done to:
- treat cancer in the small intestine, colon, rectum or anus
- treat or relieve symptoms of cancer that has spread to the intestine
- remove a blockage in the intestine (called a bowel obstruction)
- remove as much cancer as possible (called debulking)
- remove precancerous conditions before they become cancer (called prophylactic surgery)
- remove parts of the colon that are damaged by an inflammatory bowel disease or diverticulitis
- fix a tear or hole in the intestine (called a bowel perforation)
Types of bowel resections
Different types of bowel resections are done to remove different parts of the intestine. Each type of bowel resection is named based on what it removes.
Segmental small bowel resection
A segmental small bowel resection removes part of the small intestine. Some of the mesentery (a fold of tissue that supports the small intestine) and lymph nodes in the area may also be removed.
A segmental small bowel resection is used to remove tumours in the lower
part of the
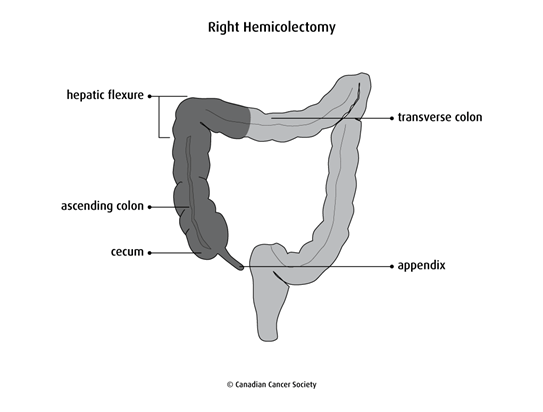
Right hemicolectomy
A right hemicolectomy removes:
- part of the ileum
-
the
cecum - the ascending colon (the first part of the colon)
- the hepatic flexure (the bend in the colon near the liver)
- the first part of the transverse colon (the middle of the colon)
- the appendix
A right hemicolectomy is used to remove tumours in the right colon, including the cecum and ascending colon. It may also be done to remove tumours of the appendix.
An extended right hemicolectomy removes all of the transverse colon. It may be done to remove tumours in the hepatic flexure or transverse colon.
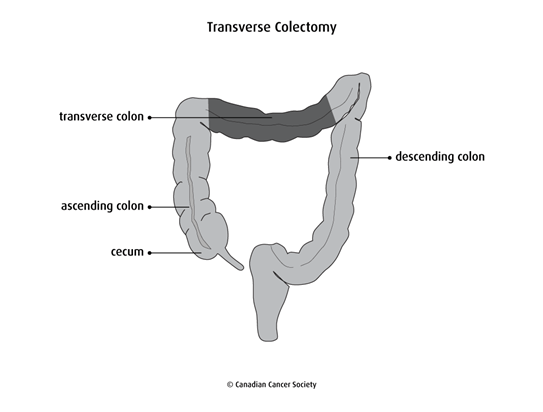
Transverse colectomy
A transverse colectomy removes the transverse colon.
This surgery may be done to remove a tumour in the middle of the transverse colon when the cancer hasn’t spread to any other parts of the colon. Sometimes an extended right hemicolectomy is done instead.
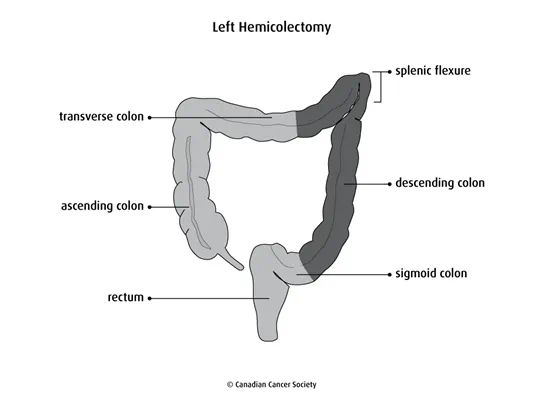
Left hemicolectomy
A left hemicolectomy removes:
- part of the transverse colon
- the splenic flexure (the bend in the colon near the spleen)
- the descending colon
- part of the sigmoid colon
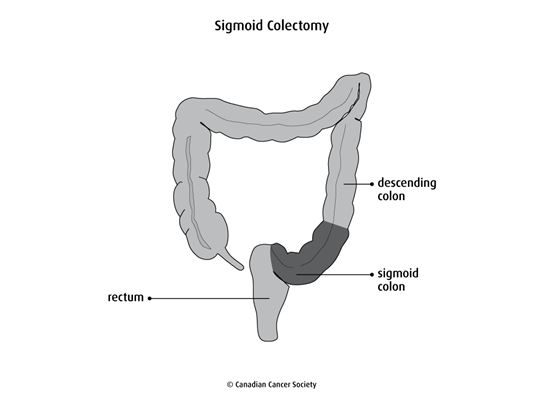
Sigmoid colectomy
A sigmoid colectomy removes the sigmoid colon. It is used to remove tumours in the sigmoid colon.
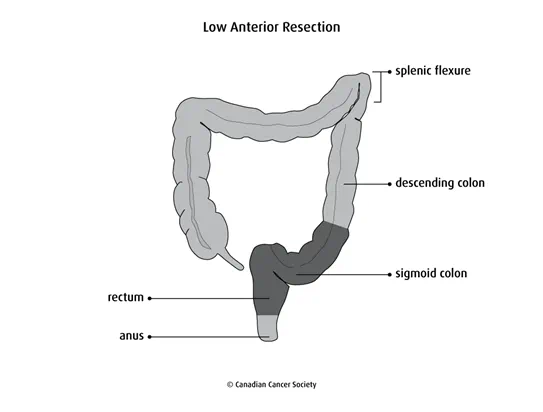
Low anterior resection
A low anterior resection removes the sigmoid colon and part of the rectum. It is used to remove tumours in the middle or upper part of the rectum.
Proctectomy with coloanal anastomosis
A proctectomy removes all of the rectum and part of the sigmoid colon. Coloanal anastomosis joins the remaining colon to the anus.
This surgery is used to remove tumours in the lower part of the rectum. Often a low anterior resection or an abdominoperineal resection is done instead.

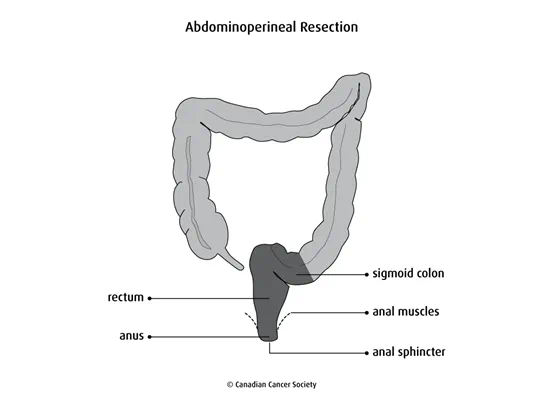
Abdominoperineal resection
An abdominoperineal resection removes the rectum, anus, anal sphincter and muscles around the anus. It is used to remove tumours that are close to the anus or have grown into the muscles around the anus.
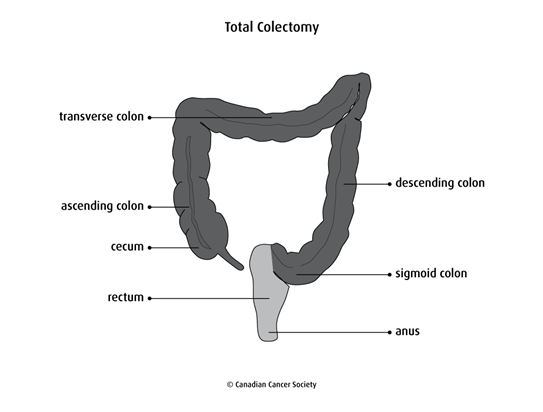
Subtotal or total colectomy
A colectomy removes part or all of the colon. If most of the colon is removed, it is called a subtotal or partial colectomy. If all of the colon is removed, including the cecum and the appendix, it is called a total colectomy.
A subtotal or total colectomy is done:
- when there is cancer on both the right and left sides of the colon
- as a way to prevent colorectal cancer (called a prophylactic colectomy) for some people with familial adenomatous polyposis (FAP) or Lynch syndrome (also called hereditary non-polyposis colon cancer or HNPCC)
- to remove a colon that is damaged by an inflammatory bowel disease
Depending on the type of colectomy done, the surgeon may also need to do a
Preparing for a bowel resection
Before surgery, tests will be done to check your general health. Blood tests, a chest x-ray and an electrocardiogram (ECG) may be done to check the health of certain organs. You may also have blood tests to check for malnutrition. If you are malnourished, your bowel resection may be postponed until your nutrition improves. Find out more about these tests and procedures and nutrition for people with cancer.
Your healthcare team will tell you if you need to follow a special diet before surgery. They will also tell you when to stop eating and drinking before surgery.
Depending on the type of bowel resection, you may need to empty your intestine before surgery. This usually means taking a laxative 1 to 2 days before surgery. You may also be given cleansing enemas at the hospital.
If you need a colostomy or an ileostomy, your surgeon will usually mark the abdomen where the stoma (opening) will be to make sure it is in a convenient and comfortable place. Your surgeon or healthcare team may also discuss the type of pouch that you will need to use after the surgery. You may be given antibiotics before surgery to help prevent infection.
Approaches to surgery
The surgeon can use an open technique or a laparoscopic technique.
- With the open technique, a large cut (incision) is made in the abdomen to reach the intestine.
-
With the laparoscopic technique, small cuts are made in the abdomen.
An
endoscope and tools are inserted through the cuts to do the surgery.
The laparoscopic technique tends to have a shorter hospital stay, faster recovery time and less pain at the incision sites. Some people may not be able to have a laparoscopic bowel resection because of the location or stage of the cancer or other factors.
How a bowel resection is done
A bowel resection is done in the hospital using general anesthesia (you will be asleep).
During a bowel resection, the surgeon removes the diseased or damaged part of the intestine. The surgeon also removes some healthy tissue on either side of the diseased or damaged part of the intestine.
Anastomosis
Once part of the intestine is removed, the 2 remaining ends of the intestine are joined together using stitches or staples. This is called an anastomosis.
When all of the large intestine is removed and the anastomosis is between the small intestine and anus, it is called an ileoanal anastomosis. When it is between the colon and anus, it is called a coloanal anastomosis.
The surgeon may form the ileum or colon into a pouch (called a J-pouch) before joining it to the anus. A J-pouch creates a holding place for stool (poop) when the rectum is removed. It helps lower the number of bowel movements the person has and manage the inability to control bowel movements.
In some cases, an anastomosis is not done. One or both ends of the intestine are attached to an opening on the abdomen instead. This procedure is called a colostomy or an ileostomy, depending on the part of the intestine used.
Lymph node dissection
If the bowel resection is being done to remove cancer, the surgeon will also remove at least 12 nearby lymph nodes. Surgery to remove lymph nodes is called a lymph node dissection.
A total mesorectal excision (TME) is a type of lymph node dissection that removes the mesorectum, which is fat surrounding the rectum that contains lymph nodes and blood vessels. A TME is usually done during a bowel resection to remove cancer in the rectum. Some tissue around the tumour is also removed.
Find out more about lymph node dissection.
Colostomy or ileostomy
Depending on which part of the intestine is diseased and how healthy the rest of the intestine is, the surgeon may need to do a colostomy or an ileostomy after a bowel resection.
A colostomy creates an opening from the colon to the outside of the body through the abdominal wall. An ileostomy creates an opening from the ileum to the outside of the body through the abdominal wall.
A colostomy or an ileostomy can be temporary or permanent. The doctor may do a temporary colostomy or ileostomy to allow the intestine to rest and heal after surgery. A colostomy or an ileostomy will be permanent if the lower part of the rectum and anal sphincter are removed during the bowel resection.
Find out more about colostomy and ileostomy.
Side effects
Side effects can happen with any type of surgery, but everyone’s experience is different. Some people have many side effects. Other people have few or none at all.
Side effects of a bowel resection are usually temporary. The side effects that you may have depend mainly on the type of bowel resection done and your overall health. Side effects of a bowel resection include:
- pain
- fatigue
- bleeding
- blood clots
- diarrhea
- constipation
- bowel obstruction
- infection
- paralyzed or inactive intestine (called paralytic ileus)
- damage to nearby organs, such as the small intestine, bladder, ureters or spleen
- leaking from where the 2 ends of the intestine were joined (called an anastomotic leak)
-
sexual problems, such as
erectile dysfunction for men or pain during sex for women - bladder problems, including the inability to control urination, the need to urinate often or an intense need to urinate
Find out more about side effects of surgery.
After surgery
After a bowel resection, you will need to stay in the hospital for several days. You will be given pain medicines to keep you comfortable. You will be offered clear fluids for 1 to 2 days after surgery. Solid foods will be introduced slowly.
You may be referred to an
If you had a colostomy or an ileostomy, a WOC (wound, ostomy and continence) nurse will teach you how to live with and care for the ostomy. Before you go home, the healthcare team or WOC nurse will talk to you about:
- changing the bandages or dressing
- showering and bathing
- how and when to take any medicines
- eating and drinking
- physical activity
- what to do if you have problems
- when to visit the surgeon for follow-up
Special considerations for children
Preparing children before a test or procedure can help lower their anxiety, increase their cooperation and develop their coping skills. This includes explaining to children what will happen during the test, such as what they will see, feel and hear.
Preparing a child for a bowel resection depends on the age and experience of the child. Find out more about helping your child cope with tests and treatments.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
