Lymph node dissection
A lymph node dissection is surgery to remove an area of lymph nodes. It is done to remove lymph nodes that have cancer and other lymph nodes when there is a very high chance that the cancer may spread there. It is also called a lymphadenectomy.
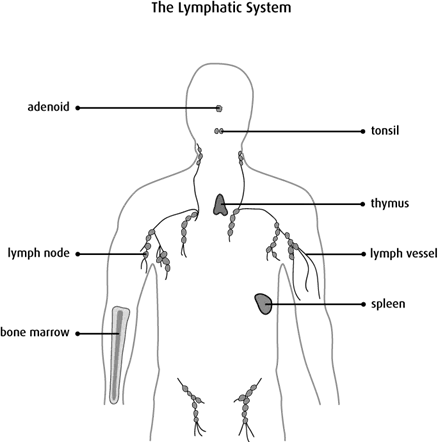
The lymph nodes are part of the lymphatic system. The lymphatic system helps fight infections and is made up of lymph vessels, lymph fluid, lymph nodes, bone marrow and the lymphatic organs (thymus, adenoid, tonsil and spleen).
Lymph vessels are very thin tubes similar to blood vessels. They collect and move lymph fluid away from tissues into the lymph nodes. Lymph nodes are small bean-shaped organs of lymphatic tissue. The lymph fluid can carry cancer cells from where the cancer started into the lymph nodes. For example, cancer cells from the breast can spread to the lymph nodes in the armpit.
Types of lymph node dissection
There are different types of lymph node dissection depending on which lymph nodes are removed.
An axillary lymph node dissection (ALND) removes lymph nodes from the armpit.
An inguinal lymph node dissection removes lymph nodes from the groin.
A neck dissection removes lymph nodes from the neck (also called cervical lymph nodes).
A
pelvic lymph node dissection (PLND)
removes lymph nodes from the pelvis in the lower
A retroperitoneal lymph node dissection (RPLND) removes lymph nodes from the back of the abdomen (retroperitoneum).
Why a lymph node dissection is done
A lymph node dissection is done to:
- check for cancer in the lymph nodes
- remove lymph nodes that may contain cancer
- reduce the risk that cancer will come back (recur)
- help doctors plan further treatment
A sentinel lymph node biopsy (SLNB) may be done before a lymph node dissection when the doctor doesn’t feel any enlarged lymph nodes. An SLNB is a simpler and safer surgery used mainly for breast cancers and melanoma skin cancers. It is done to find out if cancer has spread from a tumour to the sentinel lymph node. The sentinel lymph node is the first lymph node in a chain or group of lymph nodes that receives lymph fluid. It is the first lymph node that cancer is most likely to spread to. If doctors find cancer cells in the sentinel lymph node after they remove it, they may remove more lymph nodes from the area with a lymph node dissection.
How a lymph node dissection is done
A lymph node dissection is usually done under general
The surgeon makes a cut (incision) in the skin and removes lymph nodes and any other nearby tissue that may have cancer cells. Then the surgeon places a small tube (drain) and closes the cut with stitches or staples. A drainage bag is attached to the end of the tube to collect fluid draining from the area. This reduces the chance of fluid building up in the tissue and improves healing. The drain is left in place for a few weeks or until there is little or no drainage.
The lymph nodes and any other tissue removed during surgery are sent to a lab to be examined by a doctor who specializes in the causes and nature of disease (pathologist).
You may need to stay in the hospital for one or more days, depending on the type of lymph node dissection you have. While you are in the hospital, you may get antibiotics to prevent infection and medicine to control pain. The healthcare team will also tell you:
- how to care for and dress the wound
- how to manage the drainage bag and tube
- how much and which types of activity you can do after surgery
- how to reduce swelling
- which symptoms and side effects you should report
You will have a follow-up appointment to see the surgeon 1–2 weeks after the surgery. The surgeon will check how the wound is healing and how well you feel.
Side effects
Side effects can happen any time during, immediately after or a few days or weeks after a lymph node dissection. Sometimes late side effects develop months or years after a lymph node dissection. Most side effects go away on their own or can be treated, but some may last a long time or become permanent.
Tell the healthcare team if you have these side effects or others you think may be from a lymph node dissection:
- signs of infection, such as pain, redness, discharge or fever
- a collection of fluid under the skin (seroma) near the incision
- changes in sensation, such as pain or numbness (may happen if nerves are damaged)
- swelling due to a buildup of lymph fluid in the soft tissues (lymphedema)
The healthcare team may give you antibiotics to prevent or treat an infection, or they may drain a buildup of fluid.
The chance of developing lymphedema increases with the number of lymph nodes removed and if radiation therapy is given after a lymph node dissection. Some people have severe lymphedema. Lymphedema treatment may include massage therapy, compression garments, exercises or elevating your leg or arm to reduce swelling. Find out more about lymphedema.
What the results mean
Each lymph node removed is examined to see if it contains cancer.
- A negative lymph node has no cancer cells.
- A positive lymph node has cancer cells.
The pathologist’s report includes the type of cancer, the number of lymph nodes removed and the number of lymph nodes that have cancer cells. The report may also say if the cancer has grown through the outer covering of the lymph node (the capsule).
Doctors use the number of positive lymph nodes to help
Depending on the result, your doctor will decide if you need more tests, any treatment or follow-up care.
Special considerations for children
In rare cases, a child may need a lymph node dissection to stage or treat certain types of cancer that can spread to the lymph nodes, such as childhood breast cancer or rhabdomyosarcoma.
Preparing children before a test or procedure can lower anxiety, increase cooperation and help them develop coping skills. Preparation includes explaining to children what will happen during the test, including what they will see, feel, hear, taste or smell.
Preparing a child for a lymph node dissection depends on the age and experience of the child. Find out more about helping your child cope with tests and treatments.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
