Abnormal cervical biopsy results
After a biopsy, the tissue sample is examined under a microscope to look for changes or abnormalities such as cancer. If there are no abnormal cells, the result is reported as normal. An abnormal cervical biopsy means that there have been some changes to the cells in the cervix.
Abnormal cervical biopsy results are reported similar to abnormal Pap test results.
Describing abnormal cells in the cervix
Abnormal cells in the cervix may be described in different ways using different terms. Most often abnormal cell changes in the cervix are described using the Bethesda reporting system, which gives information about how different the cells look from normal cells. The Bethesda reporting system includes the terms low-grade squamous intraepithelial lesion (LSIL), high-grade squamous intraepithelial lesion (HSIL) and adenocarcinoma in situ (AIS). Other reporting systems refer to cervical intraepithelial neoplasia (CIN) and cervical dysplasia.
Abnormal squamous cells
This diagram shows how the different terms for describing abnormal cells in the cervix are related.
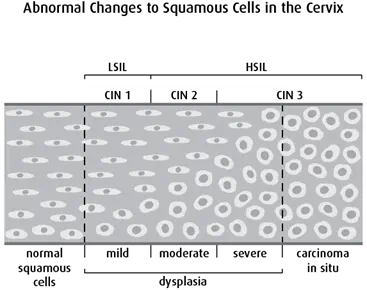
Squamous intraepithelial lesion (SIL) is the newest way of describing abnormal changes to the squamous cells in the cervix. SIL is described as low grade or high grade.
- Low-grade SIL (LSIL) compares to CIN 1 and mild dysplasia. LSIL affects a lower part of the cervical lining.
- High-grade SIL (HSIL) compares to CIN 2 and CIN 3 and moderate and severe dysplasia. HSIL affects most of the cervical lining.
Cervical intraepithelial neoplasia (CIN) is another way to describe abnormal changes to squamous cells in the cervix. Neoplasia means an abnormal and uncontrolled growth of cells.
CIN is graded on a scale of 1 to 3 based on how abnormal the cervical tissue looks under a microscope:
- CIN 1 is the least severe and compares to mild dysplasia.
- CIN 2 is moderately severe and compares to moderate dysplasia.
- CIN 3 is the most severe. It describes both severe dysplasia and carcinoma in situ (a very early stage of cancer in which tumour cells have not yet invaded surrounding tissues).
Dysplasia is another way to describe abnormal cell changes in the cervix. It means that the cells are different from normal cells in size, shape and organization within tissue. Dysplasia almost always refers to a precancerous condition.
The type of dysplasia is based on how much the abnormal cells look like normal cells:
- Mild dysplasia means the cells look slightly different from normal cells.
- Moderate dysplasia means the cells look quite different from normal cells.
- Severe dysplasia means the cells look very different from normal cells.
Abnormal glandular cells
Adenocarcinoma in situ (AIS) describes cancer cells found in the glandular tissue of the endocervix. The cancer hasn’t spread into the deeper tissues of the cervix or surrounding tissue.
Follow-up and treatment for abnormal results
Follow-up and treatment options for an abnormal cervical biopsy can vary. Depending on how severe they are, some changes or abnormalities may not need to be treated. Some abnormal cells change back to normal on their own. Other abnormal cells or precancerous changes to cells may develop into cancer if they aren’t treated.
Women with abnormal cervical biopsy results may have one or more of the following procedures for follow-up or treatment:
- A Pap test removes a small sample of cells from the cervix. Doctors examine the tissue under a microscope to see if they look normal or abnormal. Find out more about a Pap test.
- A human papillomavirus (HPV) test is used to test the cervical cells to see if they have the DNA of certain types of HPV. These high-risk types of HPV are more likely to cause cells to become cancerous. Find out more about an HPV test.
- A colposcopy uses a colposcope (a lighted magnifying instrument) to examine the vulva, vagina and cervix. During a colposcopy, the doctor may also remove cells or tissue so they can be examined under a microscope (called a biopsy).
- A biopsy removes tissues or cells from the body so they can be examined under a microscope to check for cancer. A biopsy can be done during a colposcopy. Find out more about a biopsy.
- An endocervical curettage is a type of biopsy. It uses a special tool, called a curette, to remove cells from the endocervical canal. It can be used to collect cells so they can be examined under a microscope to check for cancer. An endocervical curettage can be done during a colposcopy.
- Cryosurgery uses extreme cold (usually liquid nitrogen or carbon dioxide) to freeze and destroy abnormal cells or tissues. Find out more about cryosurgery.
- Laser surgery uses a laser, which is a high-intensity beam of light, to remove tissue. Find out more about laser surgery.
- A cone biopsy removes a cone-shaped piece of tissue from the cervix. It can be done using a surgical scalpel, loop electrosurgical excision procedure (LEEP) or laser surgery. The doctor sends the removed tissue to a lab to be examined under a microscope.
- Loop electrosurgical excision procedure (LEEP) is a type of cone biopsy. It uses a thin wire heated by an electrical current to remove tissue from the cervix. Find out more about a LEEP.
Pregnant women with abnormal cervical biopsy results
A woman who is diagnosed with LSIL when she is pregnant usually doesn’t need a repeat colposcopy or treatment until after she has her baby.
If a pregnant woman is diagnosed with HSIL, she will usually have a repeat colposcopy or treatment 8 to 12 weeks after she has her baby. Some women with HSIL will need to have more tests such as a colposcopy, a Pap test or another biopsy during pregnancy. A cone biopsy is not usually done during pregnancy because there is a small risk of bleeding.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
