Liver problems
Liver problems can develop after some types of cancer treatment. Sometimes liver problems happen as a late effect of treatments for cancer during childhood. Liver problems often develop slowly and progress gradually over time.
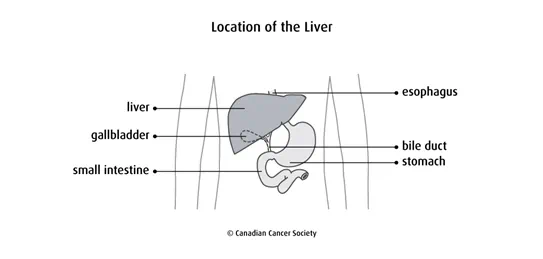
How the liver works
The liver is part of the digestive system. It is under the ribcage in the upper-right part of the abdomen. The liver makes enzymes and bile to help digest food. It also makes proteins that help the blood clot. The liver cleans the blood by removing harmful materials including chemotherapy drugs and other medicines.
Causes
Treatments for cancer, including certain types of chemotherapy, radiation therapy, immunotherapy and stem cell transplants, can cause liver problems.
Chemotherapy
Some chemotherapy drugs known to cause liver damage are:
- mercaptopurine (Purinethol)
- thioguanine (Lanvis)
- asparaginase (Kidrolase)
- carmustine (BiCNU, BCNU)
- cytarabine (Cytosar)
- methotrexate
- cisplatin
- cyclophosphamide (Procytox)
Radiation therapy
Receiving high doses of radiation to the abdomen, pelvis, spine or whole body (called total body irradiation, or TBI) can cause liver damage.
Immunotherapy
Some immunotherapy drugs, such as pembrolizumab (Keytruda), ipilimumab (Yervoy) and nivolumab (Opdivo), can cause liver damage.
Stem cell transplant
High-dose chemotherapy and total body irradiation given to prepare for a stem cell transplant can cause liver damage. Chronic graft-versus-host disease (GVHD) or veno-occlusive disease (VOD) of the liver that develops after a stem cell transplant can also cause liver damage.
Other factors
Other factors that can increase the risk of liver problems include:
- a tumour in the liver
- surgery to remove a large part of the liver
- having other conditions that affect the liver such as hepatitis
- drinking large amounts of alcohol
- having many blood transfusions
Types of liver problems
Types of liver problems that can develop following some types of cancer treatment include:
- an increase in liver enzymes with no symptoms
- an increased risk of gallstones
- an enlarged liver
- hepatitis B and C (inflammation of the liver)
-
nodules in the liver - scarring of the liver (cirrhosis)
- hardening of the liver (fibrosis)
- too much iron buildup in the body from having many blood transfusions
Symptoms
Symptoms of liver damage can vary depending on the type of problem. Sometimes liver damage doesn’t cause any symptoms. The problem may only be identified by diagnostic tests.
Symptoms of liver problems include:
- jaundice, which is yellowing of the skin and whites of the eyes
- dark urine
- pale, clay-coloured stools
- severe itching
- easy bruising or bleeding
- chronic fatigue
- pain in the abdomen
- malaise, which is a general feeling of discomfort or illness
- nausea
- loss of appetite
- an enlarged liver
- ascites, which is a buildup of fluid in the abdomen
If symptoms get worse or don’t go away, report them to your doctor or healthcare team without waiting for your next scheduled appointment.
Diagnosis
Before treatment for cancer begins, the healthcare team may do tests to check your liver and make sure there are no major problems. Tests may also be done during and after treatments to make sure nothing has changed.
Blood tests are done to:
- measure levels of enzymes that are normally present in liver cells and check how well the liver is working
- check for hepatitis
- measure blood clotting factors
- check for too much iron in the blood
Find out more about tests and procedures.
Preventing and managing liver problems
To prevent liver damage, the healthcare team carefully monitors people who are at risk. They use tests to check the liver in people receiving cancer treatment that can affect the liver. If they think the liver might be damaged, they may lower the dose of the drug or radiation or stop the treatment entirely to prevent further damage.
If you are at risk of liver damage following cancer treatment, you can help lower the risk by keeping your liver healthy.
- Get immunized against hepatitis A and B.
- Avoid alcohol or limit the amount you drink.
- Drink plenty of water.
- Eat a well-balanced diet and less fatty, salty, smoked and cured foods.
- Don’t take unnecessary medicines or more than the recommended doses of medicines.
- Don’t use illegal drugs.
- Don’t mix drugs and alcohol.
- Check with your doctor before taking any new over-the-counter medicines, herbs or supplements.
- Use barrier protection (such as condoms) during sexual contact to prevent infection by viruses that can damage the liver.
- Avoid being around chemicals that can be harmful to the liver such as solvents, aerosol cleaners, insecticides and paint thinners. Wear a mask and gloves and work in a well-ventilated area when you are around chemicals.
Follow-up
All people who are treated for cancer need regular follow-up. The healthcare team will develop a follow-up plan based on the type of cancer, how it was treated and your needs.
Make sure you tell your doctor all the treatments you received. If you are at risk for liver problems, you will have a physical exam each year to check for enlargement of the liver and blood tests to check liver function.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
