Engaging people with gene mutations to detect cancer earlier with a blood test
This project brings together a team comprised of leaders in the field of familial cancer syndromes (FCS). People with inherited, or familial, forms of cancer carry genes that place them at a high risk of developing multiple cancers throughout their lifetime, including stomach, esophageal, lung, brain and pancreatic cancers. Because of their high cancer risk, this population is regularly screened for signs of cancer and therefore represents an ideal population for the proposed clinical trials on a blood-based test for cancer, including those that are the focus of the Breakthrough Grants initiative.
The research team is building on previous work to develop a genetic blood test that can detect tumour DNA circulating in the blood stream at the same time or earlier than the conventional annual medical exams for people with FCS, when less aggressive therapies can be used, and treatments are more likely to succeed. The results of this project could have wide-reaching implications for the early detection of cancer above and beyond those people living with FCS.
Since 2017, they have been working with more than 130 clinicians, scientists and patient partners from across Canada to develop the foundation for this project. Now, with funding from the Canadian Cancer Society and the Canadian Institutes of Health Research, they are conducting a clinical trial to directly engage patient participants and prove that cancer for people with FCS at risk for high fatality cancers can be detected earlier with a simple blood test than through conventional methods.
The team has members in Canada, the United Kingdom and the United States, including 3 patient partners. If successful, this project has the potential to transform our ability to detect multiple cancers in the very early stages, revolutionizing the outcomes, access to testing and quality of life for cancer patients.
Total Amount Awarded over 5 years: $ 7,497,581.15
Team Members
- Trevor Pugh, Princess Margaret Cancer Centre - UHN, Ontario Institute for Cancer Research
- Yvonne Bombard, St. Michael's Hospital
- Raymond Kim, University Health Network
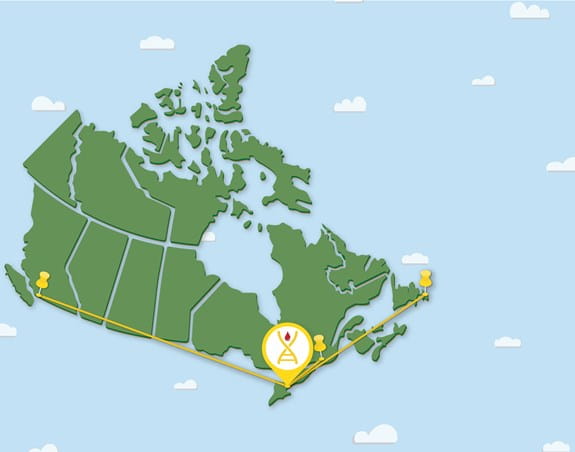
- Kasmintan Schrader, University of British Columbia
- Melyssa Aronson, Mount Sinai Hospital
- Mark Basik, Lady Davis Institute
- Julia Burnier, The Research Institute of the McGill University He
- Natalie Coburn, Sunnybrook Research Institute
- Lesa Dawson, Memorial University
- Holly Etchegary, Memorial University
- William Foulkes, McGill University
- Steven Gallinger, Mount Sinai Hospital
- Angela Hirbe, Washington University School of Medicine
- Aly Karsan, BC Cancer Agency (Vancouver)
- David Malkin, The Hospital for Sick Children
- Tracy Stockley, University Health Network
- Alicia Tone, Ovarian Cancer Canada
- Wei Xu, University Health Network
- Janice Fukakusa, Princess Margaret Cancer Foundation
- Chiquita Hessels, LFS Association Canada
- Teresa Tiano, My Gut Feeling
- Philippe Bedard, Princess Margaret Cancer Centre - UHN
- Lillian Siu, Princess Margaret Cancer Centre - UHN
- Emma Woodward, University of Manchester
Team Geography