Surgery for pituitary gland cancer
Surgery is a medical procedure to examine, remove or repair tissue. Surgery, as a treatment for cancer, means removing the tumour or cancerous tissue from your body.
Almost all pituitary gland cancers are pituitary neuroendocrine tumours (PitNETs). Most people with a PitNET have surgery. The type of surgery you have depends mainly on the size of the tumour and if it has grown into (invaded) other tissues. When planning surgery, your healthcare team will also consider other factors, such as your age and overall health.
Surgery may be the only treatment you have or it may be used along with other treatments. You may have surgery to:
- completely remove the tumour
- remove as much of the tumour as possible before other treatments
- relieve pressure from the tumour on nearby areas
- lower hormone levels and ease symptoms caused by a functioning tumour that makes too much of a certain hormone
The following types of surgery are commonly used to treat PitNETs.
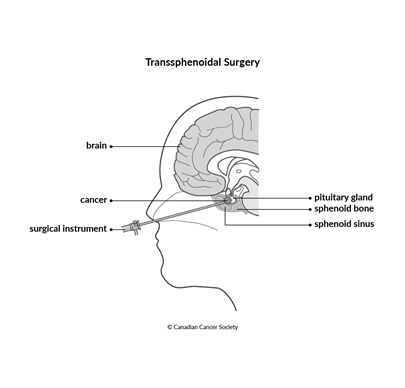
Transsphenoidal surgery
Transsphenoidal surgery is the most common type of surgery used to treat PitNETs. The surgeon reaches the pituitary gland through a hollow chamber behind the nose called the sphenoid sinus. This surgery can be used to remove some or all of a PitNET.
The surgeon makes a small cut (incision) into the cartilage and bone that separates the 2 nostrils (called the nasal septum). Using surgical tools, the surgeon goes through the sphenoid bone and sphenoid sinus to reach the pituitary gland and remove the tumour.
Endoscopic transsphenoidal surgery
is a newer technique used to remove small tumours. The surgeon makes a small
incision into the nasal septum. Then they pass an
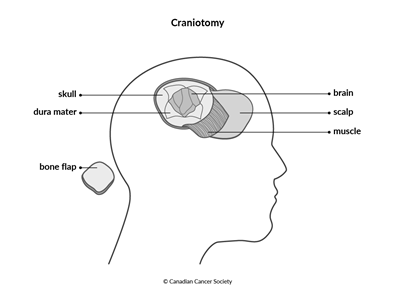
Craniotomy
A craniotomy is surgery that opens the skull to reach a tumour. It is used for tumours that can’t be removed with transsphenoidal surgery because they are very large or have grown into (invaded) other tissues.
During the surgery, the surgeon makes an incision in the scalp. A piece of the skull is removed to expose the area where the pituitary gland is. This piece of skull is often called a bone flap. The surgeon then makes an incision in the covering of the brain (called the dura mater) and pulls it apart slightly to find and reach the tumour. The surgeon removes as much of the pituitary gland tumour as possible.
Side effects
Side effects of surgery will depend mainly on the type of surgery and your overall health. Tell your healthcare team if you have side effects that you think are from surgery. The sooner you tell them of any problems, the sooner they can suggest ways to help you deal with them.
Transsphenoidal surgery may cause these side effects:
- sinus headache and congestion
-
cerebrospinal fluid (CSF) leaking from the nose - extreme thirst and the need to urinate very often (caused by arginine vasopressin deficiency, which is when low levels of the hormone vasopressin cause the body to make too much urine)
-
infection and inflammation of the
meninges (called meningitis) - vision problems or not being able to move part of the face due to damaged blood vessels, tissue or nerves near the pituitary gland
A craniotomy may cause these side effects:
- neurological problems, such as weakness, numbness, vision problems and seizures
- extreme thirst and the need to urinate very often (caused by arginine vasopressin deficiency, which is when low levels of the hormone vasopressin cause the body to make too much urine)
- fatigue, feeling cold and weight changes when the pituitary gland doesn’t make enough of 1 or more hormones (called hypopituitarism)
- bleeding in the brain
- cerebrospinal fluid (CSF) leaking from the nose
- infection
- damage to nearby blood vessels, tissue or nerves
Questions to ask about surgery
Find out more about surgery and side effects of surgery. To make the decisions that are right for you, ask your healthcare team questions about surgery.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
