Types of multiple myeloma
Multiple myeloma is the most common type of plasma cell cancer. Multiple myeloma happens when the plasma cells in the bones and bone marrow become abnormal and start to grow out of control. These abnormal plasma cells are called myeloma cells. Instead of making healthy antibodies (called immunoglobulins) to fight infections, myeloma cells produce M-proteins. M-proteins are abnormal antibodies that don't work properly. This can lead to a weakened immune system. The myeloma cells can also collect together to form tumours, called plasmacytomas, in many bones in the body.
The buildup of myeloma cells causes:
- fewer normal blood cells in the bone marrow
- weakened or damaged (fractured) bones
- bone pain
- infection
There are 2 main types of multiple myeloma – active and smouldering. Active multiple myeloma has signs and symptoms of multiple myeloma. Smouldering multiple myeloma doesn’t have signs or symptoms of the disease.
Active (symptomatic) multiple myeloma
Active, or symptomatic, multiple myeloma has signs and symptoms of multiple myeloma. It can be defined and diagnosed using a specific set of criteria. Blood and imaging tests are used to identify myeloma defining events (MDEs).
As the myeloma cells and M-proteins continue to be produced out of control and start to build up in the body, they can eventually cause symptoms related to organ damage, such as kidney damage.
Symptoms relating to organ damage caused by myeloma cells and M-proteins are grouped as CRAB symptoms. CRAB symptoms are:
- hyper c alcemia (high level of calcium in the blood)
- r enal insufficiency (kidneys not working properly)
- a nemia (low red blood cell count)
- osteolytic b one lesions (bone pain or bone fractures or both)
Other criteria or MDEs are also measured:
- Myeloma cells make up 60% or more of the blood cells in the bone marrow.
- The serum light chain ratio is 100 or greater.
- There is more than one abnormal area in the bone of at least 5 mm in size found on an MRI.
Doctors use the presence of CRAB symptoms and MDEs to indicate the disease has progressed to active multiple myeloma and active treatment should be started.
Treatment decisions are based on:
- if you can have a stem cell transplant (called transplant eligible)
- if you can't have a stem cell transplant (called transplant ineligible)
- if the cancer has returned or no longer responds to treatment (called relapsed or refractory)
Find out more about treatments for transplant eligible multiple myeloma, treatments for transplant ineligible multiple myeloma and treatments for relapsed or refractory multiple myeloma.
Smouldering (asymptomatic) multiple myeloma
Smouldering multiple myeloma is also called asymptomatic myeloma because it doesn’t cause any symptoms. This type of myeloma is a condition between a precancerous condition called monoclonal gammopathy of undetermined significance (MGUS) and active (symptomatic) multiple myeloma.
Smouldering multiple myeloma doesn't have any MDEs and has the following features:
- Myeloma cells make up 10% to 60% of the blood cells in the bone marrow.
- The M-protein level in the blood is 30 g/L or more, or the M-protein level in the urine is 500 mg or more over a 24-hour period.
Most people with smouldering multiple myeloma will eventually develop multiple myeloma with symptoms (active multiple myeloma).
If you have smouldering multiple myeloma, you will have regular tests every 3 to 6 months to see if your condition is progressing to active multiple myeloma. If the smouldering multiple myeloma is at high risk of progressing to active multiple myeloma, you may be offered treatment for multiple myeloma.
Find out more about treatments for smouldering multiple myeloma.
Other types of multiple myeloma
There are less common types of multiple myeloma.
Myeloma by immunoglobulin type
Multiple myeloma can be classified by which immunoglobulin (Ig) the myeloma cells make.
The most common types of immunoglobulins the myeloma cells make are:
- IgG (called IgG multiple myeloma)
- IgA (called IgA multiple myeloma)
The least common types of immunoglobulins the myeloma cells make are:
- IgM (called IgM multiple myeloma)
- IgD (called IgD multiple myeloma)
- IgE (called IgE multiple myeloma)
Light chain myeloma
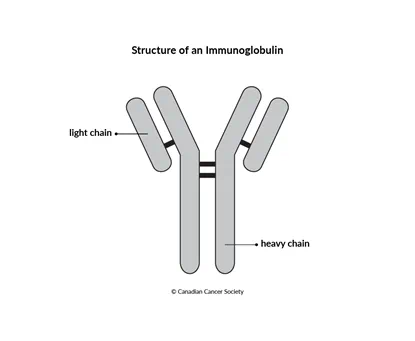
The myeloma cells of some types of multiple myeloma don’t make a complete immunoglobulin. Light chain myeloma only makes the light chain part of the immunoglobulin and not the heavy chain.
Light chains can collect in and damage the kidneys. Light chains are smaller than M-proteins and show up better in the urine than in the blood. This is because light chains are filtered out of the blood when they reach the kidneys. Light chains in urine are also called Bence-Jones proteins.
Non-secretory myeloma
The myeloma cells of some types of multiple myeloma don't release (secrete) enough M-proteins or light chains into the blood or urine to be detected by protein electrophoresis.
Non-secretory myeloma can be found in the bone marrow. X-rays will also show damaged areas of the bone (called osteolytic lesions.
Other types of plasma cell cancer
There are other types of plasma cell cancers that are similar to multiple myeloma.
Solitary plasmacytoma of the bone
A plasmacytoma develops when abnormal plasma cells (called myeloma cells) collect in one place and form a single tumour. Solitary plasmacytoma of the bone is a single tumour made up of myeloma cells found in one bone (rather than multiple tumours in different locations, as in multiple myeloma). There are no other features of multiple myeloma.
X-rays of the bones show only one damaged area of bone (called osteolytic lesion) at the location of the plasmacytoma. Myeloma cells also make up less than 10% of all of the cells in the bone marrow.
The main symptom of a solitary plasmacytoma of the bone is pain at the site of the tumour or bone breaks (fractures).
A solitary plasmacytoma is most often treated with radiation therapy.
About one-third of people with solitary plasmacytoma will eventually develop other plasmacytomas and multiple myeloma.
Find out more about radiation therapy for multiple myeloma.
Extramedullary plasmacytoma
Extramedullary plasmacytoma starts outside the bone marrow (called
extramedullary) in soft tissues of the body, such as muscles. It is most
common in areas of the upper respiratory tract, such as the throat, sinuses
around the nose (called paranasal sinuses), nasal cavity and larynx (voice
box). It may also occur in other areas, including the
A diagnosis of extramedullary plasmacytoma is made after a biopsy of the tumour. People with extramedullary plasmacytoma have normal x-rays and bone marrow biopsies. You may have an MRI or a PET scan to check other areas of the body for signs of cancer.
The symptoms of extramedullary plasmacytoma depend on where the tumour is. Because the tumour is in the soft tissue, it may press on nearby areas and cause pain or problems.
The main treatment for extramedullary plasmacytoma is radiation therapy or surgery or both.
Find out more about radiation therapy for multiple myeloma.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
