Surgery for esophageal cancer
Surgery is often used to treat esophageal cancer. The type of surgery you have depends mainly on the size, stage and location of the tumour. When planning surgery, your healthcare team will also consider other factors, such as your overall heath, your age, and whether or not you have had other surgery for esophageal cancer.
Surgery may be done for different reasons. You may have surgery to:
- completely remove the tumour
- remove as much of the tumour as possible before other treatments
- reduce pain, ease symptoms or treat blockages caused by the tumour (called palliative surgery)
Evaluation for surgery
Before surgery is offered as a treatment for esophageal cancer, your healthcare team must decide if the cancer can be removed and if you are healthy enough to have surgery.
Diagnostic tests are used to find out the size of the tumour, if the cancer has spread, where it has spread, and whether or not it can be removed with surgery.
Resectable means that a tumour can be removed with surgery. Stage 0, 1, 2 and some stage 3 cancers are usually resectable. Sometimes during surgery it's found that an esophageal cancer can't be removed because it has spread into other organs.
Unresectable means that a tumour can't be removed. Stage 4 esophageal tumours and stage 3 tumours that have spread into the nearby structures and organs are unresectable.
Inoperable means that you are not well enough to have surgery for esophageal cancer. Your healthcare team will talk to you about other treatment options.
You may also have an echocardiogram or an electrocardiogram (ECG) to look at how well your heart is working, and pulmonary function tests to check how well your lungs are working.
Getting ready for surgery
Surgery for esophageal cancer is a difficult operation that can be hard to recover from. You need to be as healthy as possible before you have surgery.
People diagnosed with esophageal cancer often have difficulty eating. Your healthcare team will check your weight and how well you have been eating. You may need nutritional supplements, a feeding tube or intravenous feeding for a few days before and after surgery to gain weight and improve your nutrition and health. You may also need antibiotics to prevent or treat infections if poor nutrition has weakened your immune system. You may be referred to a dietitian to help you with your diet before and after surgery.
If you are a smoker, it's very important to quit before surgery. Smokers have a higher risk for complications during and after surgery. And smokers don't heal as well as non-smokers after surgery. Some treatments, like chemotherapy and radiation therapy, don't work as well in smokers as they do in non-smokers.
Surgery for esophageal cancer
The following types of surgery are used to treat esophageal cancer. You may also have other treatments before or after surgery.
Esophagectomy
An esophagectomy is surgery to remove part or most of the esophagus. Sometimes a small part of the stomach is removed to get a clean margin of healthy tissue around the tumour. Lymph nodes around the esophagus are also removed during surgery.
Because the esophagus is removed, reconstructive surgery is done at the same time as the esophagectomy. Reconstructive surgery helps the gastrointestinal (GI) tract work as normally as possible after the cancer is removed.
How much of the esophagus is removed and the type of reconstructive surgery will depend on the stage of the cancer, the location and size of the esophageal tumour, and your overall health.
Tumours in the upper part of the esophagus
Surgery is not used for tumours in the upper part of the esophagus that is in the neck. These tumours are treated with chemotherapy and radiation therapy.
Tumours in the lower part of the esophagus
When an esophageal tumour is near the stomach, or in the area where the stomach and esophagus meet (gastroesophageal, or GE, junction), the surgeon will remove:
- the part of the esophagus with the tumour
- about 7 to 10 cm of normal tissue above the tumour
- part of the stomach below the tumour
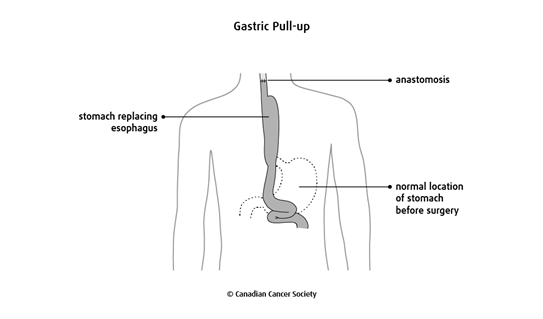
The stomach is then reshaped into a tube, pulled up into the chest or neck
area, and connected to the remaining esophagus. This is called a gastric
pull-up. The connection made between the esophagus and the stomach is called
an
Tumours in the middle part of the esophagus
Most of the esophagus is removed if a tumour is in the middle part of the esophagus. The surgeon will use a gastric pull-up to connect the stomach to the part of the esophagus left in the neck.
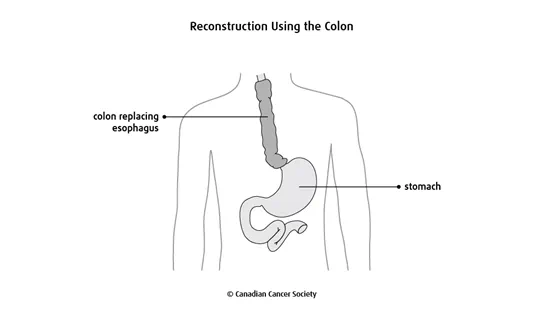
If the stomach can't be pulled up, the surgeon may use a piece of the colon (the longest part of the large intestine) or a piece of the small intestine to replace the esophagus. You may need to have this type of reconstruction if you've had stomach surgery in the past.
Surgical approaches
Surgery for esophageal cancer may be done as an open esophagectomy or as a minimally invasive esophagectomy.
Open esophagectomy
An open esophagectomy is done through large incisions (cuts). These cuts may be in different parts of the body, depending on where the tumour is in the esophagus.
A transthoracic esophagectomy removes the esophagus with incisions in the abdomen and chest.
A transhiatal esophagectomy uses incisions in the abdomen, neck and chest to remove the esophagus.
Minimally invasive esophagectomy
Minimally invasive esophagectomy is done using several small incisions.
Laparoscopic surgery is done using a long, flexible tube with a light and lens (called a laparoscope) to view structures or organs inside the body and to remove tissues. The doctor makes 4 to 6 small cuts in the abdomen to place the laparoscope.
Thoracoscopic surgery is done using a long, flexible tube with a light and lens (called a thoracoscope) to view structures and organs inside the chest, or thorax. The doctor makes small cuts through the chest wall. The thoracoscope and the surgical instruments are passed through separate cuts into the chest cavity. Sometimes doctors pass a small video camera through the thoracoscope to help them see inside the chest cavity. This is called video-assisted thoracoscopy (VAT) or video-assisted thoracic surgery (VATS).
Placement of a feeding tube
During surgery your surgeon may put a feeding tube directly into the middle part of the small intestine (called the jejunum) through an incision in the abdomen. This is called a surgical jejunostomy tube. If the tube is placed into the stomach, it's called a gastrostomy tube.
A feeding tube is used to help you to get all the nutrients you need as you recover from surgery. You will be fed by this tube for a few days after surgery because you won't be able to take in food or drinks through your mouth. Your healthcare team will do swallowing tests and x-rays to make sure the gastrointestinal (GI) tract is healed before you can drink or eat through your mouth.
Find out more about tube feeding.
Side effects
Side effects can happen with any type of treatment for esophageal cancer, but everyone's experience is different. Some people have many side effects. Other people have only a few side effects.
If you develop side effects, they can happen any time during, immediately after or a few days or weeks after surgery. Sometimes late side effects develop months or years after surgery. Most side effects will go away on their own or can be treated, but some may last a long time or become permanent.
Side effects of surgery will depend mainly on the type of surgery and your overall health.
Surgery for esophageal cancer may cause these side effects:
- pain
- bleeding
- leaking where the esophagus and stomach were rejoined (anastomotic leak)
- narrowing of the tissues where the esophagus and stomach were rejoined (anastomotic stricture)
- heartburn or bringing up (regurgitating) food or bile
- dumping syndrome
- nausea and vomiting, especially if part of the stomach was removed
- hoarseness caused by nerve damaged during surgery
- weight loss
Tell your healthcare team if you have these side effects or others you think might be from surgery. The sooner you tell them of any problems, the sooner they can suggest ways to help you deal with them.
Questions to ask about surgery
Find out more about surgery and side effects of surgery. To make the decisions that are right for you, ask your healthcare team questions about surgery.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
